Today we’re going to discuss shin pain. No, not the shin pain you get when you walk into your coffee table. And no, not the miserable shin pain we’ve all suffered from a razor scooter. We are here to talk about shin splints.
What are shin splints?

Image courtesy: https://www.medicalnewstoday.com/articles/shin-pain-not-shin-splints#minor-injury
‘Shin splints’ is a generalised term for anterior leg pain (from the ankle to the knee) induced from exercise. Pain in the shin area is commonly reported by people who engage in vigorous sporting activities such as running and jumping sport, football, soccer, and basketball.
Shin splints are caused by overuse of the muscles and bone tissue in the lower leg. The main contributing factors to the onset of shin pain includes:
- An increase in load of exercise
- Poor choice of footwear, or footwear that is unsupportive
- Poor biomechanics – foot over-pronation (inwards rolling of the ankle joint as the foot strikes the ground)
- Muscle weakness and/or inflexibility
The different types of shin splints
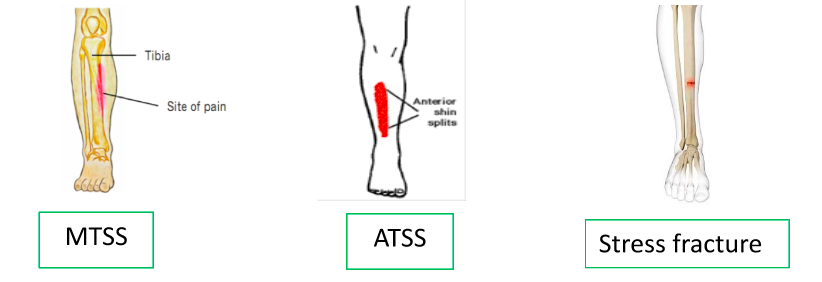
Shin splints refers to a few different conditions. Here is a quick overview of the most common ways shin splints may present:
Medial tibial stress syndrome (MTSS)
This is the most common type of shin splint, where pain on the inside edge of the tibia (shin bone) results from traction and inflammation of the posterior tibial muscles. If you run your fingers down the inside edge of your shin – it is inflammation of the bone tissue, tendons and muscles here that leads to painful symptoms. Pain with MTSS is often felt broadly.
Similar pain, but less common, can be experienced at the anterior border of the shin – anterior tibial stress syndrome (ATSS), which has very similar causes and symptoms to MTSS, just in a different location.
Stress fractures
An accumulation of repetitive stress through the tibia over time can result in a small fracture. This will often result in local pain in a much smaller area – about the size of a 20c coin – on weight bearing activity, that worsens the longer you are on your feet. Pain that is present at night would also raise suspicion for a stress fracture.
The type of shin splint you have can be diagnosed by a health care practitioner through examination, while asking all the right questions about your exercise & the location of your pain. A stress fracture can be confirmed with an MRI scan – but this is often not required.
How are shin splints treated?
For all the dedicated athletes & sports people out there, pushing through shin pain may be tempting, but it rarely results in a positive outcome. To give your injury the best outcome, book an appointment with a health care professional who can provide optimal care and management.

Dry needling treatment
An osteopath will be able to assess the injury, determine the diagnosis and address the root cause of the problem. Hands on treatment such as soft tissue massage, joint manipulation and dry needling is what we commonly offer for our patients with shin splints.
In conjunction with hands on therapy, we offer specific exercises and create a plan with you focussing on how to manage activity levels to get you back to performing your very best. In some cases, shin splints require slight de-loading from vigorous physical activity for up to 6 weeks. Of course, your normal activity may be substituted to lower impact exercise such as pilates, swimming, cycling or yoga. In less severe cases, you may be able to continue with light running, providing pain is not present during or after activity.
Bone repairs very slowly, which is why we must not rush the ‘return to running’ process. The aim is to gradually load the tibia with simple walking movements, before increasing to jogging and running eventually. When pain eases, you can increase the distance slowly. The general rule is to not increase distance or load by more than 10% per week, but may need to be more gradual depending on how your body responds.
Factors that play a role in shin pain such as running biomechanics, muscle strength, flexibility, footwear and running surface are all areas that may need to be addressed to prevent future recurrence of shin splints.
Take home tips to assist with shin splints
- Run on softer surfaces where possible (flat grass is best)
- Use appropriate footwear with plenty of support and comfort
- Perform strengthening exercises for the leg muscles – eg calf raise exercises
- Stretch the calf muscles
- Avoid making major changes to your training schedule – keep the changes gradual
- Over the counter anti-inflammatories or pain relief medication may provide temporary relief
See an osteopath at Pakenham Osteopathy to discuss further treatment and prevention options. Call 5941 4157 today or book an appointment with us online.




